Background: The extent of pretransplant workup for allogeneic hematopoietic stem cell transplant (HSCT) differs considerably among transplant centers. Current practice at the University of Wisconsin is for all recipients to undergo screening CT (computed tomography) of the sinuses, chest, abdomen, and pelvis prior to HSCT which can reveal several incidental radiographic findings. Here, we examined the impact of this procedure on discovery of clinically meaningful incidental findings, on time to transplant, on detecting post-COVID-19 infection related complications and on overall clinical outcomes post-HSCT in the current era of novel treatments for malignant hematologic disorders.
Methods: After IRB approval, all consecutive patients > age 18 years at the University of Wisconsin who underwent full body screening CT prior to HSCT, from January 2019 to August 2022 were studied. Imaging abnormalities were defined as any finding reported by the radiologist apart from isolated mucosal thickening on sinus CT scans. Post-transplant pulmonary complications were defined as abnormal chest CT scans within 6 months post-transplant. Patient and disease characteristics were tabulated, and descriptive statistics are reported. Progression free survival (PFS) is defined as the time from transplant to first identification of relapsed disease.
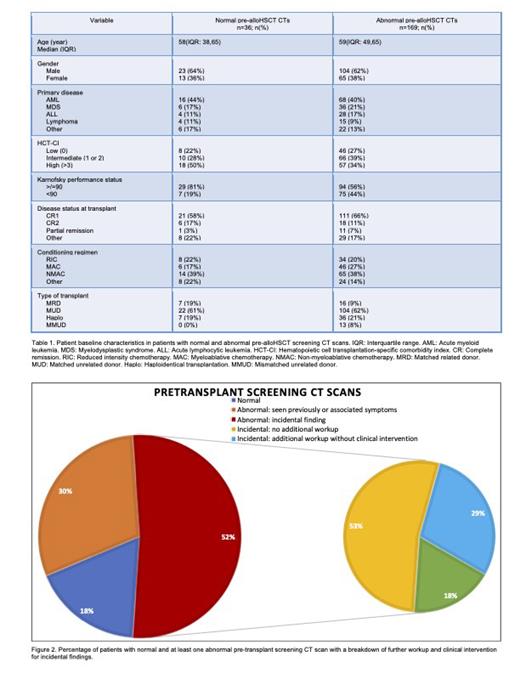
Results: Table 1 shows clinical characteristics of the study cohort. Median follow up is 22.55 months (95% CI 12.04-34.78). A total of 205 patients underwent 577 screening CT scans prior to HSCT, of which 82% (n=169) had at least one abnormal finding and 52% (n=107) had an incidental finding. Of the patients with incidental findings, 53% (n=57) received no additional workup or intervention while 47% (n=50) underwent further workup, yet only 18% (n=19) had a change in management as depicted in figure 2. Therapeutic interventions included treatment with antifungals (n=11), antibiotics (n=5), thoracentesis (n=1), thoracotomy (n=1) and anticoagulation (n=1). Although 50% of all chest CT scans identified an abnormality, only 5% revealed an incidental finding that influenced management including pulmonary nodules (n=7), bronchiolitis (n=1) and pulmonary emboli (n=1), compared to just 3% for both sinus and abdominal CT scans including sinusitis (n=4), periapical abscesses (n=3) and abdominopelvic masses of the bladder (n=1), iliac fossa (n=1), pancreas (n=1) and ovary (n=1). Post-HSCT complications were identified in 23% (n=21) vs 16% (n=15) in those with abnormal and normal pre-HSCT chest CT, respectively. In the subset of patients who underwent therapeutic interventions resulting from abnormal screening chest CT, 28% (n=5) still experienced post-transplant complications. Finally, the incidence of post-transplant pulmonary complications was similar, 27% (n=4), in patients with and without documented COVID infection prior to transplant.
Median time to HSCT after scan completion was similar in patients with normal vs abnormal imaging without additional workup at 23 days (range 11-47), compared to 24 days (range 8-62), respectively. In contrast, median time to HSCT was longer at 30 days (range 11-173) and 48 days (range 13-208) for those who received additional work up and a therapeutic intervention, respectively (p=0.0001).
One year post HSCT non-relapse mortality was 9% and 12 % among patients with normal screening CT, and those with at least one abnormal finding, respectively. 2-year PFS was similar in patients with abnormal vs normal screening chest CT scans at 60% vs 58% respectively (p=0.98).
Conclusions: We observed high rates of incidental findings leading to additional work up in over 40% of patients, though less than half of them led to changes in management. As expected, we noted a substantial risk of delay to HSCT in most recipients needing intervention. Chest CT scans had the highest prevalence of clinically significant incidental findings and meaningful impact on management, whereas routine sinus and abdomen-pelvic CT showed lower clinical benefit. No additional advantage of CT chest was found in asymptomatic patients who had a COVID-19 infection pre-HSCT. Our findings provide basis to re-evaluate current practice of pre HSCT screening, and identify at-risk patients who would benefit from screening. Additional analyses are needed to minimize risks of unnecessary interventions, delays and burden on patients and healthcare utilization.
Disclosures
Kenkre:Epizyme: Research Funding. Mattison:Nkarta: Membership on an entity's Board of Directors or advisory committees. Nadiminti:Abbvie: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal